Bone density hormones: Secrets to Optimal Bone Health 2025
Why Bone Density Hormones Matter More Than You Think
Bone density hormones are the chemical messengers in your body that control whether your bones stay strong or gradually weaken. While most people focus on calcium and vitamin D, your hormones—including estrogen, testosterone, parathyroid hormone, and several others—are actually the master regulators of bone health. They determine how quickly old bone breaks down and how efficiently new bone forms.
Key Bone Density Hormones and Their Roles:
- Estrogen – Protects bones by slowing breakdown (especially critical for women)
- Testosterone – Builds bone strength and converts to estrogen for protection (vital for men)
- Parathyroid Hormone (PTH) – Regulates calcium levels and triggers bone remodeling
- Growth Hormone & IGF-1 – Stimulates bone formation and maintains bone mass
- Thyroid Hormones (T3/T4) – Controls the speed of bone turnover
- Cortisol – When liftd, accelerates bone loss and weakens structure
The numbers tell a sobering story. In the United States alone, 44 million Americans are at risk for osteoporosis, and 10 million already have it. Women make up 80% of osteoporosis cases, and each year, 1.5 million people suffer a fracture from bone loss. What many don’t realize is that women can lose up to 20% of their bone density within the first decade post-menopause—a direct result of declining estrogen levels.
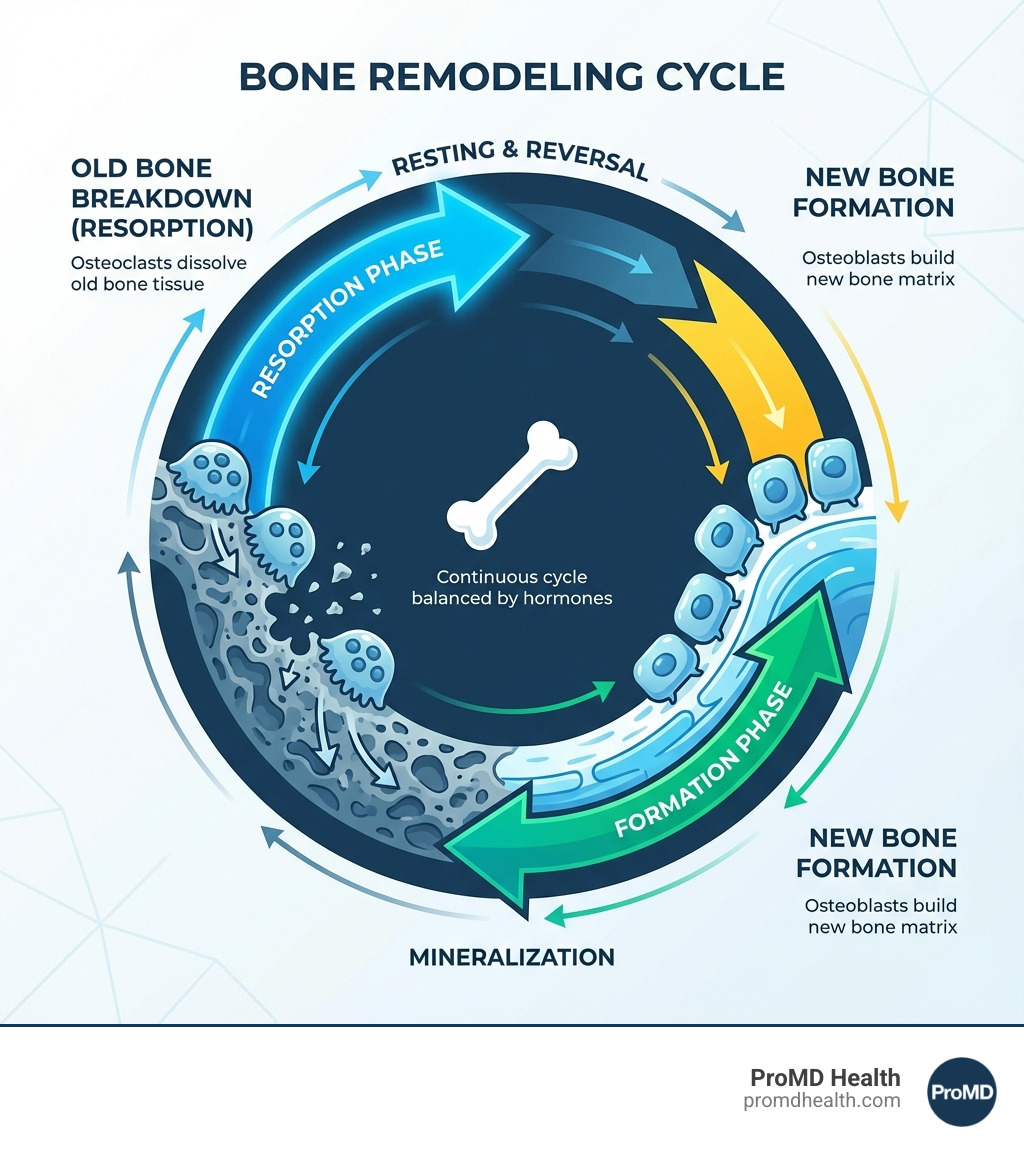
Your skeleton isn’t static. It’s a living organ that constantly breaks down old bone and builds new bone through a process called bone remodeling. This cycle repeats throughout your life, with your entire skeleton essentially renewing itself every 10 years. Two types of cells drive this process: osteoclasts (which break down old bone) and osteoblasts (which build new bone). Your hormones control the balance between these cells. When hormones are optimal, you build more bone than you lose. When hormones decline or become imbalanced—whether from aging, menopause, medical conditions, or lifestyle factors—the balance tips toward bone loss.
Bones are thickest and strongest in early adulthood, typically until your late 20s. After age 35, everyone begins to gradually lose bone mass. But this loss accelerates dramatically when key hormones shift, particularly during menopause for women or with declining testosterone in aging men.
I’m Scott Melamed, and through my work leading ProMD Health and my scientific background in biotechnology and novel drug development at Johns Hopkins, I’ve seen how understanding bone density hormones can transform preventive care and help patients maintain vitality as they age. This guide will help you understand exactly how your hormones influence your bone health—and what you can do about it.
The Key Hormonal Players in Bone Health
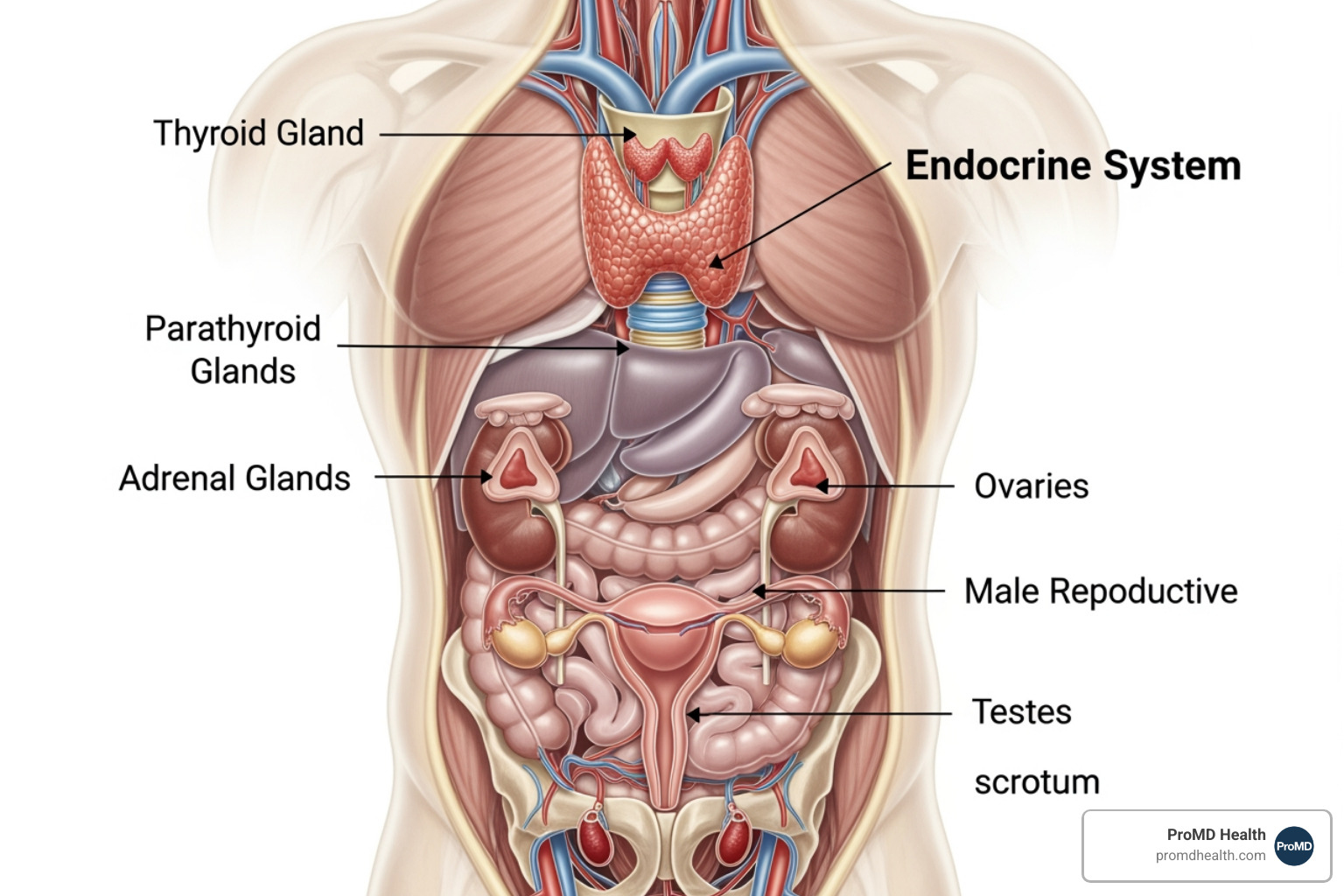
Our endocrine system is a complex network of glands that produce and secrete hormones, acting as the master conductors of our body’s functions, including bone metabolism. This intricate process involves a delicate balance between bone formation by osteoblasts (our bone-building cells) and bone resorption, or breakdown, by osteoclasts (our bone-resorbing cells). When this balance is maintained, we enjoy strong, healthy bones. However, when our bone density hormones are out of sync, it can lead to significant bone loss and increased fracture risk.
Estrogen: The Guardian of Female Bone Density
Estrogen is arguably the most critical hormone for maintaining bone density in women, acting as a powerful guardian of our skeletal health. Its primary protective role is to inhibit the activity of osteoclasts, reducing bone resorption. When estrogen levels are adequate, bone formation generally outpaces bone breakdown, keeping our bones strong.
However, the natural decline in estrogen levels during perimenopause and especially after menopause dramatically shifts this balance. This is why women make up 80% of osteoporosis cases, and why we often see a rapid decrease in bone density during this life stage. In fact, women can lose up to 20% of their bone density within the first decade post-menopause. This accelerated bone loss occurs because lower estrogen levels lead to increased osteoclast activity and a longer lifespan for these bone-resorbing cells. Estrogen also plays a crucial role in regulating the RANKL pathway, a key signaling system that controls osteoclast formation and function. Understanding estrogen’s critical role in bone homeostasis is fundamental to addressing female bone health challenges. For more scientific details, you can explore scientific research on estrogen’s role in bone homeostasis.
Testosterone: The Foundation of Male Bone Strength
While often associated with male virility, testosterone is just as vital for bone health in men, and surprisingly, also plays a significant role in women’s bone density. In men, testosterone directly promotes bone formation by stimulating osteoblasts and reduces bone breakdown. It also contributes to bone strength by undergoing a process called aromatization, where it’s converted into estrogen in bone tissue. This estrogen then exerts its protective effects, similar to its role in women.
As men age, their testosterone levels naturally decline, a process sometimes referred to as andropause. This age-related decrease in testosterone contributes significantly to bone loss in men after 65 years of age, increasing their risk of osteoporosis. Additionally, testosterone helps maintain muscle mass, which is crucial for supporting the skeleton and preventing falls. Low testosterone can lead to various symptoms, including reduced bone density. If you’re experiencing Symptoms Low Testosterone or wonder Do I Have Low Testosterone?, it’s important to understand What Causes Low Testosterone and the Common Symptoms of Low Testosterone in Men. Ignoring it can lead to serious health issues, so addressing What Happens If Low Testosterone Goes Untreated? is vital. We offer solutions to Address Low Testosterone Washington DC – Promd Health and can guide you through The Power of Testosterone Therapy and its Unexpected Benefits of Hormone Replacement Treatment for Men. For more information, explore our resources on Symptons Low Testosterone Levels Men, Are You Suffering From Low T?, How Can You Fix Low Testosterone?, and how to Take the Next Step with Male Hormone Optimization.
The Supporting Cast: Other Essential Bone Density Hormones
Beyond sex hormones, several other key players orchestrate bone health:
- Parathyroid Hormone (PTH): Produced by the parathyroid glands, PTH’s primary role is to maintain stable calcium levels in our blood. If blood calcium drops too low, PTH signals the bones to release calcium into the bloodstream. While essential for calcium homeostasis, chronically high PTH levels can lead to excessive bone resorption and weakening of bones over time.
- Vitamin D (Calcitriol): Technically a hormone, not just a vitamin, Calcitriol (the active form of Vitamin D) is crucial for bone health. It helps our bodies absorb calcium from the gut, ensuring that enough calcium is available for bone formation. Vitamin D also directly influences osteoblasts and osteoclasts, contributing to bone remodeling and overall bone mass.
- Calcitonin: This hormone, produced by the thyroid gland, acts in opposition to PTH. It helps protect against excessive blood calcium by inhibiting osteoclast activity and promoting calcium deposition into bones.
- Growth Hormone (GH) and IGF-1: Growth hormone, secreted by the pituitary gland, is fundamental for bone growth and development during childhood and adolescence. In adulthood, GH, along with its mediator Insulin-like Growth Factor 1 (IGF-1), continues to play a vital role in maintaining bone density and stimulating bone formation. Declining IGF-1 levels with age are associated with lower bone mineral density and increased fracture risk.
- Thyroid Hormones (T3/T4): These hormones are essential for normal skeletal development and bone maintenance. However, an imbalance can be detrimental. Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can negatively impact bone density. Excess thyroid hormone can accelerate bone turnover, leading to more bone loss than formation.
- Cortisol: Our primary stress hormone, cortisol, produced by the adrenal glands, has a complex relationship with bone. While necessary for many bodily functions, chronically liftd cortisol levels are detrimental to bone health. Cortisol directly inhibits osteoblast activity, reduces bone formation, and can increase bone resorption. This is a significant factor in conditions like glucocorticoid-induced osteoporosis, a common secondary cause of bone loss. An in-depth look at this can be found in an update on glucocorticoid-induced osteoporosis.
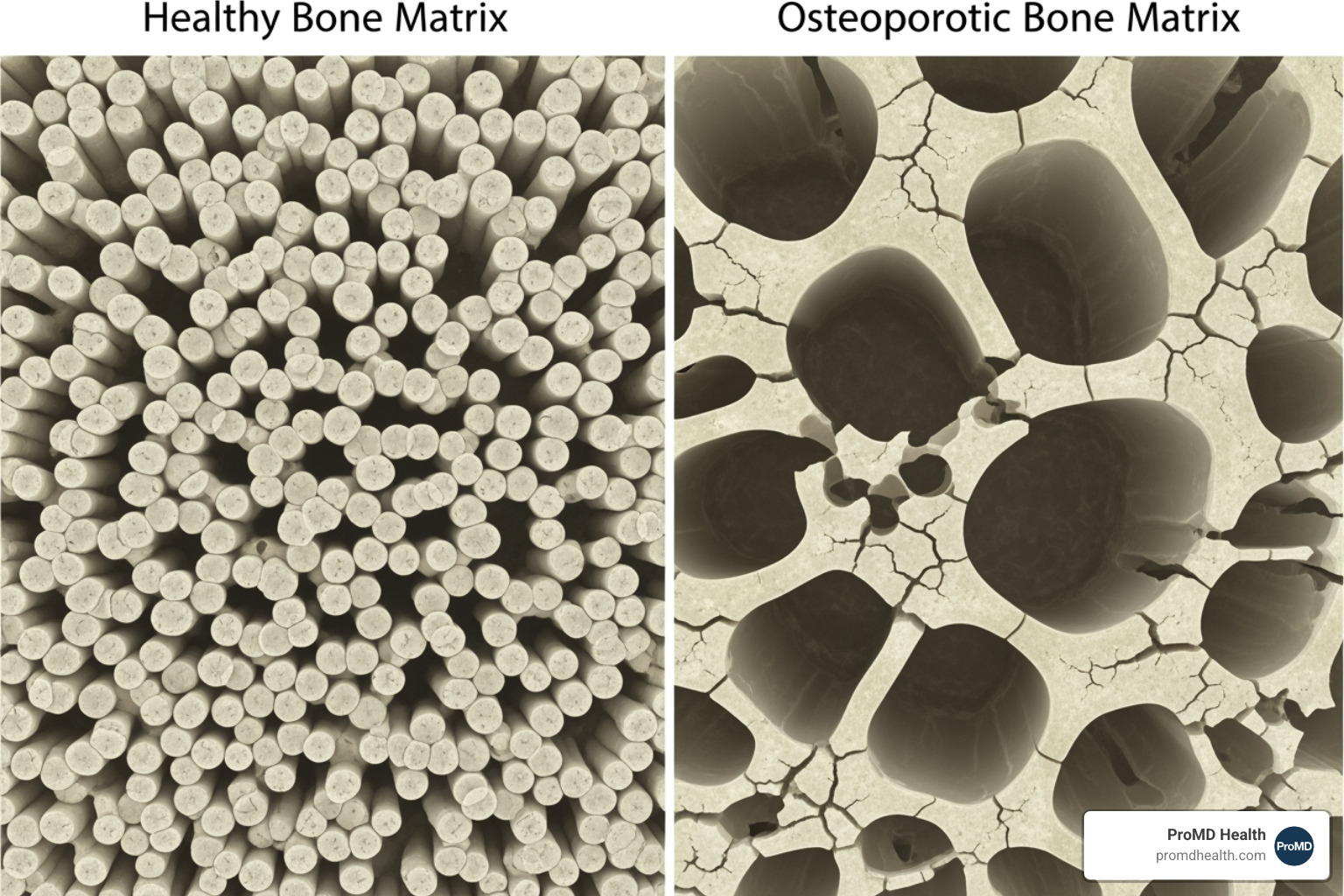
When the Balance Shifts: How Your Bone Density Hormones Affect Osteoporosis Risk
Osteoporosis is a progressive condition characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to bone fragility and a significantly increased fracture risk. It literally means “porous bone.” The diagnosis is often made based on Bone Mineral Density (BMD) measurements, typically using a DEXA scan, with a T-score of -2.5 or less indicating osteoporosis. When our bone density hormones fall out of their delicate balance, the scales tip towards increased bone resorption and decreased bone formation, paving the way for this silent disease.
Unpacking Your Risk: Hormonal and Non-Hormonal Factors
Understanding your risk factors is the first step in proactive bone health management. These factors can be broadly categorized into hormonal and non-hormonal influences:
-
Hormonal Factors:
- Menopause: As we’ve discussed, the significant drop in estrogen during menopause is a primary driver of bone loss in women. Early menopause (before 45) or a hysterectomy before 45 (especially with ovary removal) dramatically increases this risk. Even absent periods for more than 6 months due to over-exercising or dieting can lower estrogen and impact bone density.
- Low Testosterone: For men, low levels of testosterone, whether due to aging or conditions like hypogonadism, contribute to weaker bones.
- Thyroid Disease: Both an overactive (hyperthyroidism) and underactive (hypothyroidism) thyroid can negatively affect bone health.
- Cushing’s Syndrome: This condition, caused by prolonged exposure to high levels of cortisol, leads to significant bone damage.
- Hyperparathyroidism: Overactivity of the parathyroid glands results in chronically liftd PTH, drawing calcium from the bones.
- Pituitary Gland Disorders: Disorders of the pituitary gland can trigger osteoporosis due to imbalances in hormones like growth hormone or those affecting sex hormone production.
- Certain Cancer Treatments: Some treatments for breast and prostate cancer can lower sex hormone levels, increasing osteoporosis risk.
-
Non-Hormonal Factors:
- Age: Bone loss naturally accelerates with age; osteoporosis-associated fractures are increasingly prevalent in women after 55 years of age, as well as in men after 65 years of age.
- Gender: Women are at a higher risk, accounting for 80% of osteoporosis cases.
- Family History: A parental history of hip fracture or a family history of osteoporosis increases your susceptibility.
- Body Frame Size: Individuals with small, thin body frames tend to have less bone mass to begin with.
- Ethnicity: Caucasian and Asian individuals generally have a higher risk.
- Long-term Use of Certain Medications: High-dose steroid tablets (glucocorticoids) are a common culprit.
- Eating Disorders: Conditions like anorexia nervosa can lead to significantly reduced sex hormone production and severe bone loss.
- Lifestyle Choices: Heavy drinking, smoking, and a lack of physical activity are all detrimental.
- Rheumatoid Arthritis: This inflammatory condition can increase osteoporosis risk.
- Inactivity/Bed Rest: Prolonged periods of inactivity lead to rapid bone loss.
The Impact of Chronic Conditions on Bone Health
Several chronic health conditions can also disrupt hormonal balance and contribute to bone loss, often through complex pathways:
- Diabetes: Both type 1 and type 2 diabetes have been linked to reduced bone quality and increased fracture risk. Insulin, a hormone that influences bone growth, can be dysregulated in diabetes, impacting bone health.
- Chronic Liver Disease: Liver diseases can impair vitamin D metabolism, reduce the production of bone-building proteins, and lead to hormonal imbalances, all contributing to bone loss. For more on this, refer to Bone diseases in patients with chronic liver disease.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis are associated with increased osteoporosis risk due to chronic inflammation, malabsorption of nutrients (like calcium and vitamin D), and often, the use of corticosteroids. A comprehensive review highlights this link in Systematic review of the prevalence and development of osteoporosis or low bone mineral density and its risk factors in patients with inflammatory bowel disease.
- Celiac Disease: This autoimmune disorder causes malabsorption in the small intestine, leading to deficiencies in essential bone nutrients like calcium and vitamin D, and can indirectly affect hormonal balance.
- Malabsorption Syndromes: Any condition that interferes with nutrient absorption can starve your bones of the building blocks they need, leading to weaker bones.
Lifestyle’s Role: How Your Habits Influence Your Hormones and Bones
We often underestimate the power of our daily choices, but lifestyle medicine is a potent tool for maintaining bone health and hormonal harmony. Our diet, exercise routines, and stress management techniques directly influence our bone density hormones and, consequently, our skeletal strength. It’s truly amazing how much control we have over our preventative health.
Fueling Your Frame: Diet and Nutrition for Hormonal Harmony
What we eat directly impacts our hormone production and bone health. Think of your plate as a prescription for stronger bones:
- Calcium: The most abundant mineral in bone. We need 1,000-1,200 mg daily (under age 50) and 1,200 mg daily (after age 50).
- Vitamin D: Crucial for calcium absorption. Recommendations are 400-800 IU daily (under age 50) or 800-1,000 IU daily (after age 50).
- Magnesium: Involved in over 300 biochemical reactions, including bone formation.
- Vitamin K2: Directs calcium to bones and away from arteries.
- Protein Intake: Essential for bone matrix formation.
- Phytoestrogens and Isoflavones: Found in foods like soy, these plant compounds can mimic estrogen’s bone-protective effects, particularly beneficial for postmenopausal women.
- Mediterranean Diet: This anti-inflammatory eating pattern, rich in fruits, vegetables, whole grains, and healthy fats, has been linked to improved bone mineral density. A systematic review on this topic is available in Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: a systematic review and meta-analysis of observational studies.
- Omega-3 Fatty Acids: These healthy fats, found in fish and flaxseed, have anti-inflammatory properties that can indirectly support bone health.
Move It or Lose It: Exercise for Stronger Bones
Our bones respond to physical stress by becoming stronger. Regular physical activity, especially specific types, is non-negotiable for robust skeletal health:
- Weight-Bearing Exercise: Activities where you bear your own weight, like walking, jogging, dancing, and hiking, stimulate bone-building cells.
- Resistance Training: Lifting weights or using resistance bands puts stress on muscles, which in turn pulls on bones, promoting increased density. High-Intensity Resistance and Impact Training (HiRIT) has shown significant promise. For example, High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial demonstrated positive effects.
- Balance Exercises: Tai chi and yoga improve balance, reducing the risk of falls—a major cause of fractures in individuals with weakened bones.
Habits that Harm: Smoking, Alcohol, and Chronic Stress
Some lifestyle choices actively work against our efforts to maintain healthy bones:
- Smoking: Tobacco use can lower estrogen levels in women, increase cortisol, and reduce blood supply to bones, all contributing to bone loss.
- Excessive Alcohol Consumption: Heavy drinking can interfere with calcium and vitamin D absorption, disrupt hormonal balance, and increase the risk of falls.
- Chronic Stress: Sustained psychological stress lifts cortisol levels. As we discussed, high cortisol directly inhibits osteoblast activity, impairs bone formation, and can accelerate bone breakdown. This constant physiological burden can significantly impact bone density over time. Emerging research, such as Potential mechanisms linking psychological stress to bone health, highlights the intricate connection between our mental state and skeletal health. Techniques like mindfulness-based stress reduction can help regulate cortisol, indirectly benefiting our bones.
Modern Strategies for Managing and Improving Bone Density
Proactive management of bone health involves a multi-faceted approach, combining diagnostic tools, medical interventions, and emerging therapies. Our goal at ProMD Health is to help you steer these options to ensure your bones remain strong and resilient for years to come. For a comprehensive overview, we often refer to resources like The clinician’s guide to prevention and treatment of osteoporosis.
Medical Interventions and Monitoring
- DEXA Scans: Dual-energy X-ray absorptiometry (DEXA) is the gold standard for measuring bone mineral density (BMD) and diagnosing osteoporosis. We typically recommend DEXA scans for women over 65 and younger individuals with significant risk factors.
- Hormone Replacement Therapy (HRT): For women, HRT, particularly bioidentical hormone replacement therapy (BHRT), can be a highly effective strategy to counter estrogen-related bone loss post-menopause. HRT can significantly slow bone loss and maintain or even increase bone density, reducing the risk of hip and vertebral fractures. We specialize in personalized BHRT to help you Feel Younger and Regain Your Equilibrium with Hormone Replacement Therapy. Learn more about 3 Things to Know About Bio-Identical Hormone Replacement Therapy and how it can Increase Energy Levels: Bio-Identical Hormone Replacement. We also offer HRT Telehealth services.
- Bisphosphonates: These are a class of drugs that slow down bone breakdown, helping to preserve existing bone density.
- Anabolic Agents: Medications like teriparatide (a form of PTH) stimulate new bone formation, effectively rebuilding bone structure.
- SERMs (Selective Estrogen Receptor Modulators): These drugs, such as raloxifene, act like estrogen in some tissues (like bone) while blocking its effects in others, offering bone protection without some of the risks associated with traditional estrogen therapy.
At ProMD Health, we provide comprehensive Hormone Optimization Therapy custom to your individual needs. We help you understand How Does Hormone Optimization Work? and How Long Does Hormone Optimization Therapy Take to Work?. Our goal is for you to Feel Better Naturally through Bioidentical Hormone Replacement Therapy and specialized Services: Menopause Management and Services: Hormone Imbalance. We address Common Questions About a Hormonal Imbalance and offer Services: Longevity & Functional Medicine.
The Future of Bone Health: Emerging Research on Bone Density Hormones
The field of bone health is constantly evolving, with exciting new research shedding light on novel hormonal pathways and their therapeutic potential:
- The Gut-Bone Axis: Our gut microbiome is increasingly recognized as a significant player in overall health, including bone density. Research suggests a direct link, where gut bacteria produce compounds like short-chain fatty acids (SCFAs), such as butyrate, which can influence bone metabolism. Studies indicate that butyrate is necessary for parathyroid hormone (PTH) to effectively stimulate bone formation, highlighting a fascinating interplay between our gut and our skeleton. This is explored further in Research on gut microbiota and PTH-dependent bone formation.
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH): Traditionally known for their roles in reproduction, FSH and LH are now being investigated for direct effects on bone. Emerging evidence suggests that FSH may actively stimulate osteoclast activity and bone resorption, independent of estrogen levels. This opens new avenues for therapeutic targets, particularly for postmenopausal osteoporosis.
- Leptin: This hormone, primarily known for regulating appetite and energy balance, also influences bone metabolism. Research is ongoing to fully understand its complex role, which can involve both positive and negative effects on bone density depending on the context.
These emerging areas promise a future where we can better understand and target the intricate hormonal symphony that governs our bone health.
Frequently Asked Questions about Bone Density and Hormones
Can I improve my bone density after menopause?
Yes, through a combination of diet, targeted exercise like resistance training, and medical therapies if necessary. It’s absolutely possible to slow bone loss and even build new bone. The key is a personalized approach that addresses your specific hormonal profile and lifestyle.
Does stress really affect my bones?
Yes, chronic stress significantly impacts your bones. Persistent elevation of the hormone cortisol directly interferes with bone-building cells (osteoblasts), suppressing their activity. It also accelerates bone breakdown by osteoclasts, leading to lower bone density over time. Managing stress is a crucial,, component of bone health.
Are there natural ways to balance my bone density hormones?
Absolutely! Lifestyle changes can significantly help. A nutrient-rich diet (emphasizing calcium, vitamin D, magnesium, and vitamin K2), regular weight-bearing and resistance exercise, stress management techniques (like yoga or meditation), and adequate sleep can all support healthier hormone levels and optimize bone metabolism naturally.
Conclusion
We’ve journeyed through the intricate world of bone density hormones, uncovering their profound influence on our skeletal health. From the protective accept of estrogen and testosterone to the critical roles of PTH, Vitamin D, growth hormone, thyroid hormones, and the subtle yet impactful effects of cortisol, it’s clear that calcium alone is just one piece of a much larger puzzle. Your hormones are the master architects, constantly working to maintain the dynamic balance of bone remodeling.
We’ve also seen how age, gender, chronic conditions, and especially our daily lifestyle choices—what we eat, how we move, and how we manage stress—can either support or sabotage this delicate hormonal symphony. The good news is that with modern strategies, including advanced diagnostics like DEXA scans and personalized medical interventions like Hormone Replacement Therapy, alongside powerful lifestyle modifications, we have more tools than ever to manage and improve bone density.
At ProMD Health, we believe that understanding your bone density hormones is a key pillar of graceful aging and overall vitality. By optimizing your hormonal balance, we can help you not only protect your bones but also improve your energy, mood, and overall well-being. Our commitment is to empower you to look younger and feel younger, ensuring your skeletal framework remains strong for all of life’s adventures.
To learn more about how we can help you optimize your hormones and support your bone health, we invite you to explore our comprehensive range of services. Learn more about our wellness and anti-aging services and take the first step towards a stronger, healthier you.