Progesterone therapy benefits: Crucial for 2025 Wellness
Why Progesterone Matters for Your Health and Vitality
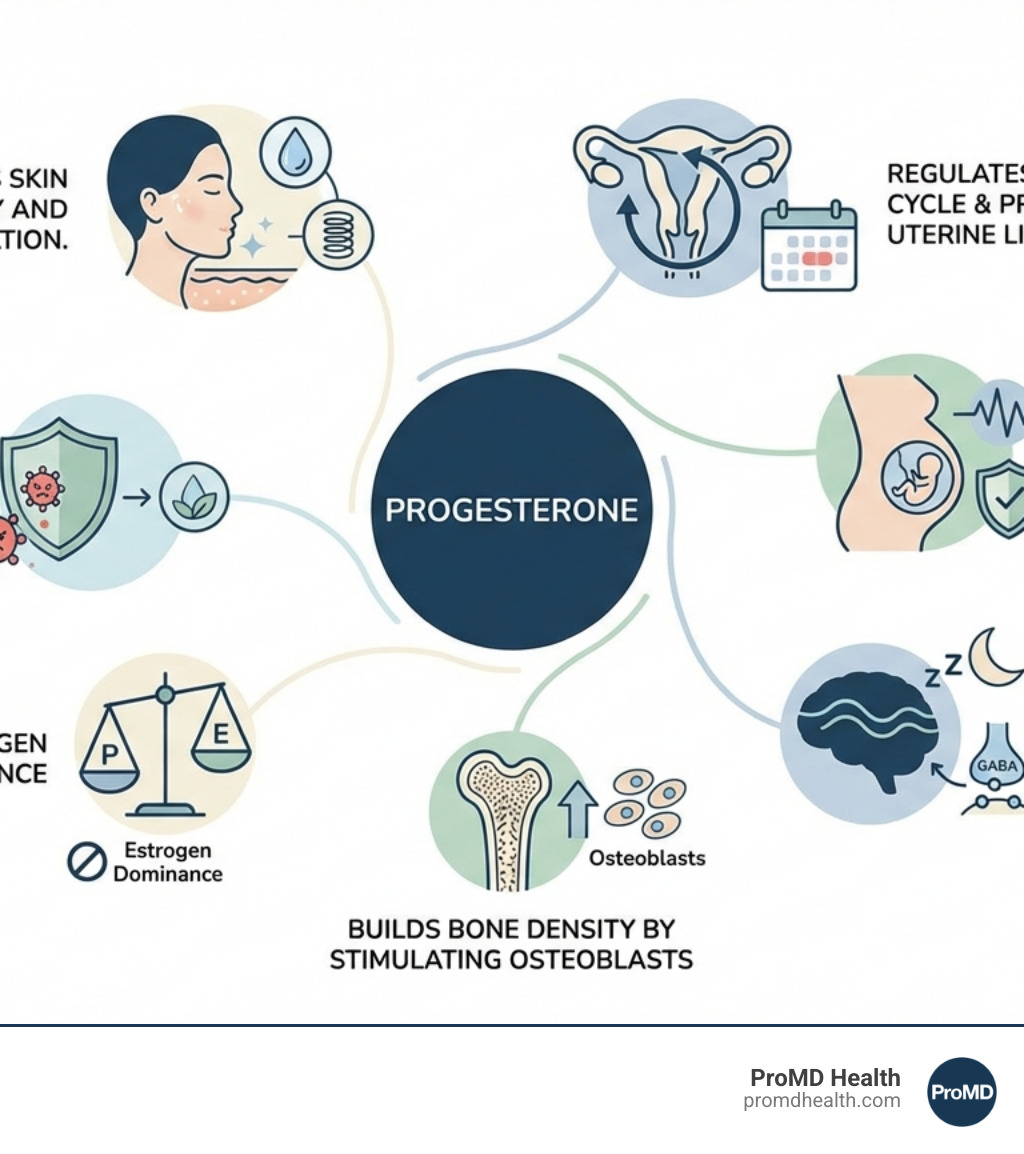
Progesterone therapy benefits extend far beyond pregnancy support—this often-overlooked hormone plays a crucial role in sleep quality, mood stability, bone health, skin vitality, and overall hormonal balance, especially as you steer perimenopause and menopause.
Key Benefits of Progesterone Therapy:
- Protects the uterus when taking estrogen in hormone replacement therapy
- Improves sleep quality through calming effects on the brain
- Stabilizes mood and reduces anxiety by interacting with GABA receptors
- Supports bone health by stimulating bone-building cells
- Improves skin elasticity and hydration for a more youthful appearance
- Reduces histamine response, helping with allergies and inflammation
- Balances estrogen to prevent hormonal dominance
Progesterone is sometimes called the “feel-good” hormone because of its natural calming and mood-stabilizing properties. Your body produces it primarily after ovulation, but levels naturally decline with age—particularly during perimenopause and menopause. This decline can trigger a cascade of symptoms including sleep disturbances, mood swings, irregular periods, and increased anxiety.
The good news? Understanding progesterone’s role and exploring bioidentical progesterone therapy can help restore balance and vitality.
An important distinction: Research shows that natural, bioidentical progesterone has a significantly better safety profile than synthetic progestins. The E3N Study found that transdermal estrogen plus progesterone did not increase breast cancer rates (RR: 1.08), while synthetic progestins showed hazard ratios of 1.23 to 2.0 in other major studies. This difference matters tremendously for your long-term health.
I’m Scott Melamed, President and CEO of ProMD Health, and my background in biotechnology from Johns Hopkins University and research in hormone-related conditions has given me deep insights into how progesterone therapy benefits can transform health outcomes for individuals seeking to optimize their wellness and vitality. My mission is to help you understand the science behind feeling your best at every age.
Understanding Progesterone’s Natural Role
Think of progesterone as your body’s master regulator—a steroid hormone that does so much more than its name suggests. While “pro-gestation” literally means “for pregnancy,” this hormone orchestrates a symphony of functions throughout your body, from your monthly cycle to your brain chemistry.
Your ovaries produce progesterone primarily after ovulation, and understanding how this works helps explain why you might feel different at various times of the month—and why things change as you age.
Every month during your reproductive years, progesterone levels rise and fall in a carefully choreographed dance. After ovulation releases an egg, the leftover follicle in your ovary transforms into something called the corpus luteum—essentially a temporary hormone factory that pumps out progesterone.
This surge of progesterone has a specific mission: preparing your uterine lining for a potential pregnancy. It transforms the endometrium from a growing phase to a nurturing phase, creating the perfect environment for a fertilized egg to implant. If pregnancy happens, progesterone levels stay liftd, supporting those crucial early weeks.
But here’s what many people don’t realize: progesterone is also your body’s natural check on estrogen. It prevents the uterine lining from growing too thick, which is essential for preventing endometrial hyperplasia—a condition where excessive tissue buildup can lead to serious problems. This balancing act between estrogen and progesterone is fundamental to uterine health.
The Menstrual Cycle and Pregnancy
The moment ovulation occurs, your progesterone story begins. The corpus luteum becomes your body’s progesterone powerhouse, and its work is nothing short of remarkable.
During the luteal phase of your cycle, progesterone transforms your uterine lining into a thick, nutrient-rich environment—think of it as preparing a cozy nest. If conception occurs, progesterone becomes the guardian of early pregnancy. It prevents uterine contractions that could threaten the developing embryo, keeping everything calm and stable during those vulnerable first weeks.
But progesterone’s influence reaches far beyond your reproductive organs. As a neurosteroid, it affects your brain and nervous system in profound ways. It influences mood, cognition, and sleep patterns—which explains why you might feel more relaxed or sleep better during certain parts of your cycle, or why you might experience mood shifts when progesterone levels drop.
This brain connection is why many women notice they feel calmer and sleep more soundly during the second half of their cycle when progesterone peaks. It’s not your imagination—it’s biochemistry.
Why Progesterone Declines
As you move through your late 30s and 40s, progesterone is often the first hormone to start declining. This happens gradually during perimenopause, sometimes years before menopause actually begins.
The main culprit? Anovulatory cycles—months when your ovaries don’t release an egg. No egg release means no corpus luteum forms, and without the corpus luteum, there’s no progesterone surge. These cycles become increasingly common as ovarian function naturally changes with age.
Chronic stress throws another wrench into the works. When you’re under constant pressure, your body prioritizes making cortisol (your stress hormone) over progesterone. This “pregnenolone steal” phenomenon means the raw materials that could become progesterone get diverted to stress management instead. It’s your body choosing immediate survival over long-term balance.
The symptoms of low progesterone can sneak up on you, and they’re surprisingly varied. You might notice irregular or unusually heavy periods, or have trouble sleeping even when you’re exhausted. Mood changes like increased anxiety, irritability, or unexplained sadness can appear. Some women experience hot flashes and night sweats—often mistaken as purely estrogen-related, but actually caused by the imbalance when progesterone drops while estrogen remains relatively high.
If you’re trying to conceive, low progesterone can make it difficult to get pregnant or maintain early pregnancy.
Recognizing these signs is crucial because they signal that your hormonal balance has shifted. Understanding this is the first step toward exploring whether progesterone therapy benefits might help restore your vitality and well-being.
Open uping Progesterone Therapy Benefits for Menopause and Beyond
When progesterone levels start to drop during perimenopause and menopause, many women find themselves struggling with symptoms they never experienced before. Hot flashes interrupt important meetings. Sleep becomes elusive. Mood swings feel unpredictable and overwhelming. This is where Hormone Replacement Therapy (HRT) can make a profound difference—and progesterone is often the missing piece of the puzzle.
Progesterone therapy benefits women navigating menopause in multiple ways. It helps manage those uncomfortable symptoms—the night sweats, the mood fluctuations, the sleepless nights. But perhaps even more importantly, it addresses a common hormonal imbalance called estrogen dominance. This happens when estrogen levels remain relatively high while progesterone declines, creating an imbalance that can amplify menopausal symptoms and health risks.
For women with a uterus who need estrogen therapy, progesterone isn’t just helpful—it’s essential. Estrogen alone causes the uterine lining to grow thicker and thicker, increasing the risk of endometrial hyperplasia and potentially uterine cancer. Progesterone acts as a protective guardian, promoting the healthy shedding of this lining and keeping your uterus safe. This endometrial protection is one of the most critical progesterone therapy benefits in HRT.
| Feature | Natural Micronized Progesterone | Synthetic Progestins (e.g., MPA) |
|---|---|---|
| Molecular Structure | Identical to the progesterone produced by the human body | Chemically altered versions; different molecular structures |
| Source | Derived from plant sources (e.g., yams, soy) and micronized for better absorption | Artificially manufactured |
| Metabolism | Metabolized into beneficial neurosteroids (e.g., allopregnanolone), often contributing to calming effects and improved sleep | Metabolized differently, can produce varying effects and side effects due to different receptor affinities |
| Endometrial Protection | Highly effective in preventing endometrial hyperplasia, as shown in studies like PEPI | Also effective in endometrial protection, but with a different side effect profile |
| Breast Health | Studies suggest neutral or antiproliferative effects on breast tissue; E3N study showed no increased breast cancer risk (RR: 1.08 with transdermal estrogen) | Linked to increased breast cancer risk in some major studies (WHI: 1.23, Million Women Study: 2.0) |
| Cardiovascular Effects | Generally neutral or positive effects on lipid profiles (e.g., less impact on HDL-C than MPA); KEEPS reported protective effects | Can have adverse effects on lipid profiles (e.g., negating estrogen’s positive effect on HDL-C); associated with increased cardiovascular risks in some studies |
| CNS Effects | Calming, anxiolytic, sedative effects; improves sleep and mood | Less pronounced or different CNS effects; can sometimes lead to mood disturbances |
| Side Effects | Common side effects can include drowsiness (often why it’s taken at night), dizziness, breast tenderness. Generally well-tolerated. | Broader range and often more severe side effects, including mood changes, bloating, and potential cardiovascular/cancer risks. |
Balancing Estrogen and Protecting the Uterus
Think of estrogen and progesterone as dance partners in HRT—they work best when they’re in sync. Estrogen does wonderful things for menopausal symptoms, helping with hot flashes, vaginal dryness, and bone health. But when given alone to a woman who still has her uterus, estrogen can overstimulate the endometrial lining, causing it to grow too thick. This condition, called endometrial hyperplasia, is a precancerous state that no one wants to deal with.
Progesterone changes everything. It transforms the uterine lining from a growth phase to a secretory phase, and ultimately helps it shed in a healthy way. The landmark PEPI trial demonstrated this beautifully—micronized progesterone, taken once daily for 12 days each month at bedtime, protected the endometrium from hyperplastic changes just as effectively as synthetic progestin therapies, but with a better overall safety profile.
This protective role is a cornerstone progesterone therapy benefit. It means you can safely experience the symptom relief that estrogen provides while keeping your uterine health intact. That’s what we mean by achieving true hormonal harmony—both hormones working together to support your wellbeing.
Natural vs. Synthetic: A Critical Distinction
Here’s where things get confusing, and honestly, a bit frustrating. The words “progesterone,” “progestogen,” and “progestin” get thrown around interchangeably, but they’re not the same thing at all. Understanding the difference could be one of the most important health decisions you make.
Bioidentical progesterone, also called micronized progesterone, is molecularly identical to what your ovaries naturally produce. It’s derived from plant sources like yams or soy, then processed to match your body’s own progesterone molecule for molecule. Because of this identical structure, your body recognizes it and uses it exactly as it would its own hormone.
Synthetic progestogens—commonly called progestins—are a different story. Medications like medroxyprogesterone acetate (MPA) are chemically altered versions of progesterone. Scientists changed their molecular structure, which means they behave differently in your body. They bind to different receptors, follow different metabolic pathways, and can produce very different effects and side effects compared to natural progesterone.
Yes, synthetic progestins can protect the endometrium. But their broader impact on your body—on your breasts, your cardiovascular system, your mood—can differ dramatically from bioidentical progesterone. For a deeper understanding of these differences and what they mean for your safety, we encourage you to read this scientific research on hormone safety. The choice between natural and synthetic isn’t just technical—it’s deeply personal and consequential for your long-term health.
Understanding the Safety Profile: More Progesterone Therapy Benefits
If you’ve heard scary stories about HRT, you’re not alone. The Women’s Health Initiative (WHI) study in 2002 sent shockwaves through the medical community and left many women confused and frightened about hormone therapy. The study reported increased risks of breast cancer and blood clots with HRT, leading countless women to abandon treatments that were helping them feel like themselves again.
But here’s the critical context that often gets lost: the WHI study primarily used synthetic progestins—specifically MPA—combined with conjugated equine estrogens. The findings reflected the risks of that specific combination, not of all hormone therapy, and certainly not of bioidentical progesterone.
Since then, research has painted a much more reassuring picture for natural progesterone. The differences are striking. While the WHI study showed a breast cancer hazard ratio of 1.23 with synthetic progestins, and the Million Women Study reported a ratio of 2.0, the E3N Study told a completely different story. When women used transdermal estrogen with natural progesterone, there was no increase in breast cancer rates (RR: 1.08). Laboratory studies have even shown that progesterone has antiproliferative or neutral effects on breast cancer cells, while synthetic progestins like MPA can stimulate cell growth.
The cardiovascular news is equally encouraging. The PEPI trial found no increase in blood pressure in women taking estrogen with progesterone compared to those taking placebo. Even better, progesterone had minimal impact on the positive effects estrogen has on HDL cholesterol (the good kind), while medroxyprogesterone significantly reduced this benefit. The KEEPS Reports from 2011 went further, showing that progesterone had protective effects for the cardiovascular system and cognitive function, with no increased risk of breast cancer, stroke, heart attack, or blood clots compared to placebo.
The E3N cohort study reinforced these findings—women receiving progesterone in hormone therapy showed no increase in breast cancer rates or blood clot risks compared to women not receiving hormone treatment at all.
These research findings reveal profound progesterone therapy benefits that extend far beyond symptom management. Natural progesterone offers a safety profile that makes it possible for many women to confidently pursue hormone therapy as part of their wellness journey, helping them feel vibrant and healthy through menopause and beyond.
The Wide-Ranging Health Advantages of Progesterone
When most people think about progesterone, pregnancy and menstrual cycles come to mind. But here’s what’s truly fascinating: this remarkable hormone influences virtually every system in your body, from your brain chemistry to your bone density. Understanding these broader progesterone therapy benefits can be genuinely life-changing, especially if you’ve been struggling with issues that seem unrelated to hormones.
Beyond supporting reproductive health, progesterone acts as a powerful neuroprotective agent, shielding your brain cells from damage and supporting cognitive function. It also works throughout your body as an anti-inflammatory compound, helping to calm chronic inflammation that contributes to aging and disease. These effects ripple outward, touching everything from how well you sleep to how resilient your immune system is.
Key Progesterone therapy benefits for Mood and Sleep
If you’ve ever noticed that you sleep better or feel calmer during certain weeks of your cycle, you’ve experienced progesterone’s influence firsthand. This hormone has a profound calming effect on your brain, which is why many women describe it as nature’s own anti-anxiety medication.
Here’s how it works: Progesterone interacts directly with GABA receptors in your brain. GABA is your primary “calm down” neurotransmitter—it acts like a brake pedal for your nervous system, slowing down overactive brain activity. When progesterone improves GABA’s effects, you experience reduced anxiety, less mental chatter, and a genuine sense of relaxation. This isn’t just feeling slightly less stressed; it’s a biochemical shift that helps your entire nervous system settle.
For sleep, the impact can be transformative. Many women going through perimenopause and menopause struggle with insomnia—lying awake at night, mind racing, unable to find that peaceful drift into sleep. Progesterone’s sedative properties help you not only fall asleep more easily but also achieve deeper, more restorative sleep cycles. This is why many healthcare providers recommend taking progesterone at bedtime. You’re working with your body’s natural rhythms rather than against them.
The mood benefits extend beyond just anxiety reduction. Progesterone helps stabilize the emotional ups and downs that can accompany hormonal fluctuations, particularly the irritability and mood swings associated with PMS. When your progesterone levels are balanced, you’re likely to feel more emotionally steady, less reactive, and better equipped to handle daily stressors.
Bone, Skin, and Immune Health
The physical benefits of progesterone extend from your skeleton to your skin—and even to how your immune system responds to the world around you.
For your bones, progesterone plays an active construction role. While estrogen helps prevent bone breakdown, progesterone actually stimulates osteoblasts—the specialized cells that build new bone tissue. Think of it this way: estrogen protects what you have, but progesterone helps you build more. This dual action is particularly important as you age and your natural bone density begins to decline. Maintaining adequate progesterone levels can be a key strategy in preventing osteoporosis and keeping your skeletal system strong and resilient.
Your skin tells the story of your hormonal balance, and progesterone contributes significantly to that radiant, healthy glow. This hormone supports collagen production, which keeps your skin supple and elastic. With balanced progesterone, you may notice improved skin hydration, better texture, and even a reduction in fine lines. It’s not magic—it’s simply giving your body the hormonal tools it needs to maintain healthy skin from the inside out.
One of the most underappreciated progesterone therapy benefits involves histamine regulation. If you’ve been dealing with mysterious headaches, skin flushing, seasonal allergies that seem worse than they should be, or digestive discomfort, histamine intolerance might be playing a role. Here’s the connection: estrogen tends to increase histamine production and release, while progesterone helps counterbalance this effect.
Progesterone works by stabilizing mast cells—the immune cells that release histamine when triggered. By keeping these cells calmer and less reactive, progesterone helps reduce the overall histamine load in your body. For women with histamine intolerance, this can mean fewer headaches, less skin irritation, reduced allergy symptoms, and better overall comfort. It’s particularly relevant during perimenopause when progesterone naturally declines while estrogen levels may still fluctuate wildly, creating a perfect storm for histamine-related issues.
These diverse benefits—from stronger bones to healthier skin to a calmer immune response—demonstrate that progesterone truly is a whole-body hormone. When we talk about looking younger and feeling younger, these are the biological mechanisms that make it possible.
Navigating Progesterone Therapy Safely
Starting on any hormone therapy journey requires careful consideration and personalized guidance. At ProMD Health, we emphasize that navigating progesterone therapy safely means a highly individualized approach, always beginning with a comprehensive medical consultation. Our goal is to ensure that the treatment aligns perfectly with your unique health needs and goals.
During your consultation, we’ll discuss your medical history, current symptoms, and lifestyle. We’ll also consider the most appropriate dosing and administration routes for progesterone, which can vary. Options include oral capsules (often taken at night for their sedative effect), vaginal inserts, or transdermal creams. The choice of route can impact how the hormone is metabolized and its effects on your body.
Potential Side Effects and Contraindications
While natural micronized progesterone is generally well-tolerated, it’s important to be aware of potential side effects and situations where it might be contraindicated.
Common side effects can include:
- Drowsiness or fatigue (often why it’s recommended at bedtime)
- Dizziness
- Headaches
- Breast tenderness or pain
- Nausea or gastrointestinal upset
- Mood changes (though often positive, some may experience shifts)
More serious, though less common, side effects warrant immediate medical attention. These include signs of blood clots (pain in the chest, groin, or legs; sudden shortness of breath; slurred speech), sudden severe headache, or vision changes.
Progesterone therapy may be contraindicated or require extreme caution in individuals with:
- A history of certain cancers (e.g., breast cancer, unless specifically managed by an oncologist)
- Liver disease or impaired liver function
- Unexplained vaginal bleeding
- A history of blood clots or stroke
- Active cardiovascular disease
Always discuss your full medical history with your healthcare provider to determine if progesterone therapy is right for you.
Progesterone Intolerance: Signs and Management
Occasionally, individuals may experience what we call progesterone intolerance, where their body reacts negatively to progesterone or progestogens. This can manifest as symptoms that mimic PMS, such as:
- Bloating
- Increased breast tenderness
- Irritability or heightened emotional sensitivity
- Negative mood shifts, including increased anxiety or depression
- Fatigue that feels worse rather than better
If you suspect you’re experiencing progesterone intolerance, it’s crucial to work closely with your healthcare provider. Management often involves adjusting the dosage of progesterone. Sometimes, a lower dose is all that’s needed to alleviate symptoms. Another effective strategy can be changing the administration route. For instance, if oral progesterone causes significant drowsiness or mood changes due to its metabolites, switching to vaginal progesterone might be beneficial. Vaginal administration often delivers progesterone more directly to the uterus with less systemic absorption, potentially reducing systemic side effects. Your healthcare provider can help you explore these options and find a regimen that works best for your body.
Conclusion
Throughout this journey, we’ve explored how progesterone serves as far more than just a pregnancy hormone. It’s truly a multifaceted player in your overall health and vitality. From regulating your menstrual cycle and protecting your uterus to calming your mind for better sleep, strengthening your bones, enhancing your skin’s glow, and even helping manage histamine responses—the progesterone therapy benefits touch nearly every aspect of how you feel day to day.
What matters most, though, is understanding that not all progesterone is created equal. The research is clear and compelling: bioidentical progesterone offers a significantly safer profile than synthetic progestins, especially when it comes to breast cancer risk and cardiovascular health. The E3N Study’s findings—showing no increased breast cancer risk with natural progesterone compared to the liftd risks seen with synthetics—should give you confidence that choosing the right form of hormone therapy can make a real difference in your long-term wellness.
This isn’t about accepting symptoms as an inevitable part of aging. It’s about reclaiming your vitality and feeling like yourself again. At ProMD Health, we don’t believe in one-size-fits-all solutions. Your hormonal landscape is as unique as you are, which is why we create personalized wellness plans that harness the power of bioidentical progesterone therapy to help you look younger and feel younger. Whether you’re navigating perimenopause, managing menopausal symptoms, or simply seeking to optimize your hormonal balance, we’re here to guide you with expertise rooted in science and delivered with care.
If you’re ready to explore how balanced hormones can transform your energy, mood, sleep, and overall well-being, we’d love to help you take that next step. Our team serves communities throughout Maryland, Virginia, Florida, Texas, Colorado, Delaware, and the District of Columbia—including Annapolis, Arlington, Ashburn, Bel Air, Bethesda, Columbia, Easton, Fort Lauderdale, Hutto, Lafayette, Lewes, Timonium, Tysons Corner, Washington, Wellington, and Westminster.
Find how our comprehensive approach to hormonal health fits into your wellness journey. More info about our anti-aging and wellness services.