Hrt meaning: Ultimate 2025 Guide for Safe HRT
Understanding Hormone Replacement Therapy: What You Need to Know
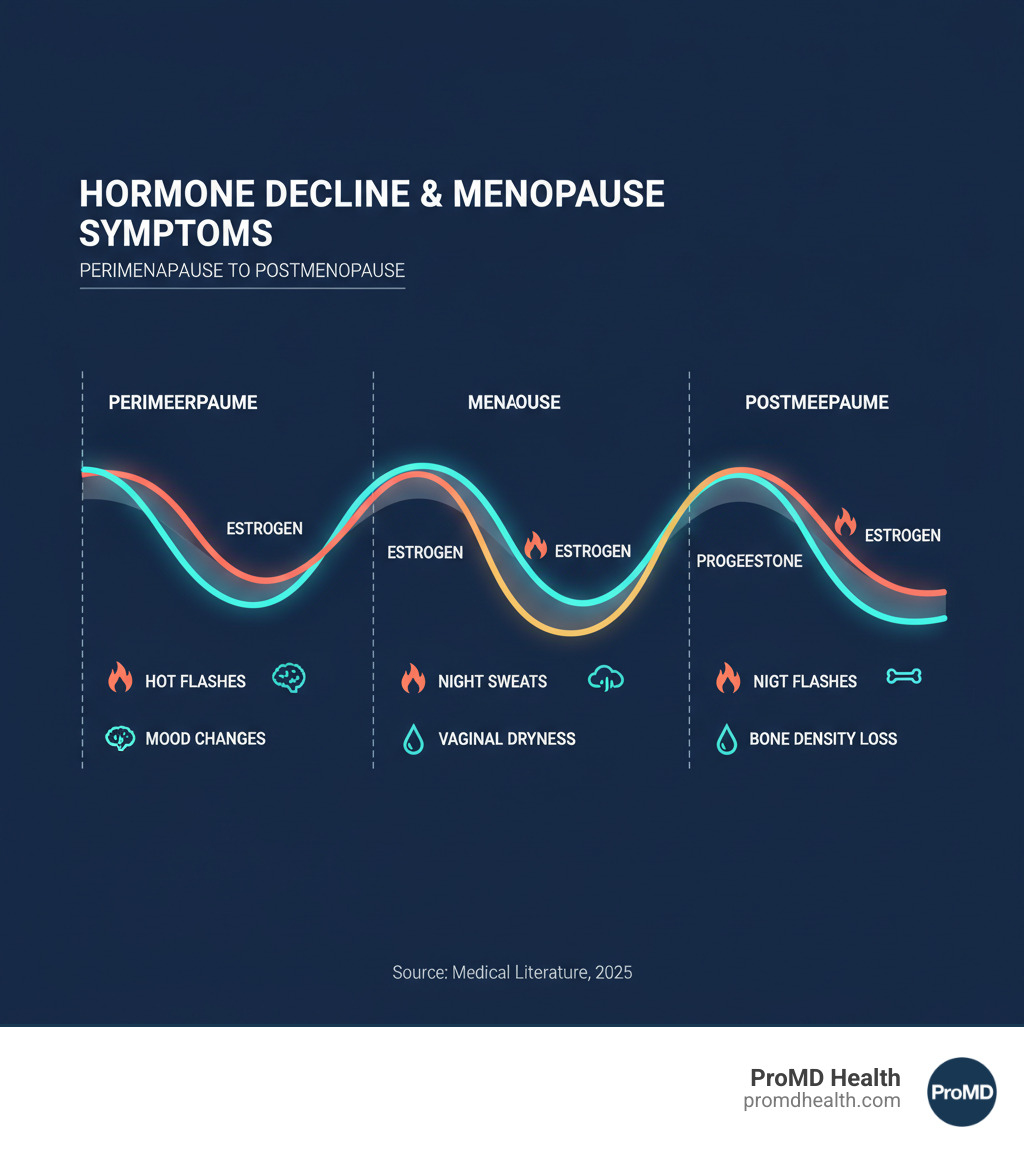
The HRT meaning refers to Hormone Replacement Therapy, a medical treatment that replaces hormones—primarily estrogen and progesterone—that decline during menopause. Also known as Menopausal Hormone Therapy (MHT), it is the most effective treatment for relieving symptoms like hot flashes, night sweats, vaginal dryness, and sleep disturbances, while also helping protect against bone loss.
If you’re struggling with menopausal symptoms that impact your daily life, you’re not alone. Yet many women remain confused about what HRT is and whether it’s right for them. The conversation around HRT has been complex, especially after the Women’s Health Initiative (WHI) study in the early 2000s caused a dramatic drop in its use.
Today, medical experts have a much clearer understanding of HRT’s benefits and risks. Current evidence shows that for most healthy women under 60 who start therapy within 10 years of menopause, the benefits often outweigh the risks. However, the decision is deeply personal and depends on your health history, symptoms, and goals.
As Scott Melamed, President of ProMD Health, I’ve seen how understanding the true hrt meaning can transform women’s health and quality of life. This guide will explain HRT, helping you make an informed choice about whether it’s right for you.
What is Hormone Replacement Therapy (HRT)?
Think of Hormone Replacement Therapy (HRT) as a way to restore what your body loses during menopause. Also called Menopausal Hormone Therapy (MHT), it’s a medical treatment that supplements the hormones—primarily estrogen and progestogen (a form of progesterone)—that naturally decline as you transition through perimenopause and menopause. Sometimes testosterone is also included to address low energy and libido.
The goal isn’t just replacing hormones; it’s about helping you feel like yourself again by restoring balance and relieving the often-debilitating symptoms of menopause that can impact work, relationships, and overall quality of life.
What is the clinical hrt meaning for menopause?
Clinically, the hrt meaning for menopause is centered on symptom management. Menopause is natural, but suffering through its symptoms doesn’t have to be. HRT effectively addresses:
- Hot flashes and night sweats: Sudden, intense waves of heat that disrupt daily activities and sleep, leading to exhaustion and affecting mood and concentration.
- Vaginal dryness (Genitourinary Syndrome of Menopause – GSM): As estrogen drops, vaginal tissues become thinner and drier, causing discomfort, pain during intercourse, and a higher risk of urinary tract infections.
- Mood swings and brain fog: Hormonal shifts can cause irritability, anxiety, and frustrating cognitive issues like poor concentration and memory lapses.
By restoring hormone levels, HRT can provide dramatic, life-changing relief from these symptoms.
What are the long-term health considerations?
Beyond daily symptom relief, HRT plays a key role in long-term health, particularly for your bones.
One of its most significant benefits is osteoporosis prevention. Estrogen is vital for maintaining bone density, and its decline during menopause accelerates bone loss. HRT slows this process, keeping bones stronger and reducing fracture risk.
This protection is especially crucial for women who experience premature menopause (before age 40) or early menopause (between 40 and 45). For these women, HRT is considered essential therapy to prevent the serious long-term consequences of prolonged estrogen deficiency, such as osteoporosis and heart disease. Scientific research on premature menopause confirms that HRT offers vital protection.
The relationship between HRT and cardiovascular health is nuanced. While not prescribed solely for heart disease prevention, studies show that when started within 10 years of menopause or before age 60, it does not increase cardiovascular risk and may even be protective. Timing is critical, as starting HRT later in life has been linked to increased risks. At ProMD Health, we emphasize individualized care to steer these important decisions.
The Benefits vs. Risks: A Deep Dive into HRT
Deciding on HRT can feel overwhelming, with conflicting stories from friends and family. Understanding the hrt meaning for your personal health requires weighing both sides of the equation with a healthcare provider who knows your medical history.
For many women, the benefits are life-changing. They include powerful symptom relief from hot flashes and night sweats, leading to improved sleep quality. HRT also provides crucial bone protection against osteoporosis, helps stabilize mood swings, maintains skin elasticity, and can restore sexual function by addressing vaginal dryness and improving libido.
The Landmark Women’s Health Initiative (WHI) Study
Much of the fear surrounding HRT traces back to the 2002 Women’s Health Initiative (WHI) study. Initial reports highlighted increased risks of breast cancer, heart disease, and stroke, causing panic and a sharp decline in prescriptions.
However, the crucial context often missed was that the study participants were, on average, 63 years old—well past the typical age for starting HRT. Subsequent re-evaluation of the data led to the “timing hypothesis”: when you start HRT matters. For healthy women who begin therapy within 10 years of menopause or before age 60, the benefits generally outweigh the risks. This re-evaluation has restored HRT as a valuable and safe option when used appropriately.
Understanding the Potential Risks and Side Effects
HRT is not risk-free. The risks depend on the type of hormone, dose, delivery method, and your personal health history.
- Blood clots (VTE) and stroke: The risk is small and primarily associated with oral estrogen. Transdermal forms (patches, gels) carry a much lower risk.
- Breast cancer: Estrogen-only therapy shows a neutral or even reduced risk. Combined estrogen-progestogen therapy may slightly increase risk after about five years of use, but this risk decreases after stopping HRT.
- Endometrial cancer: This risk is increased by taking estrogen alone. It is why progestogen is always prescribed for women with a uterus, as it protects the uterine lining.
Common side effects like bloating, breast tenderness, or headaches are usually mild and often resolve within a few months. At ProMD Health, we monitor these effects and adjust treatment to ensure your comfort.
How to Minimize HRT Risks
Fortunately, risks can be minimized with a strategic approach:
- Use the lowest effective dose for the shortest appropriate duration needed to manage symptoms.
- Choose transdermal (skin) application over oral pills to lower the risk of blood clots.
- Use micronized progesterone if progestogen is needed, as it may have a better safety profile.
- Maintain regular medical follow-ups to reassess your treatment plan.
- Adopt healthy lifestyle habits, including exercise, a balanced diet, and avoiding smoking.
For more detailed guidance, The American College of Obstetricians and Gynecologists provides evidence-based recommendations, such as their ACOG guidelines on HRT and Heart Disease.
Navigating Your HRT Journey: Types, Timing, and Candidacy
Finding the right HRT approach is a personalized process. Your journey is shaped by your body, symptoms, and health history. At ProMD Health, we believe the best plans come from careful assessment and conversation.
Different Types of HRT Available
The type of HRT you use depends on whether you have a uterus.
- Estrogen-Only Therapy: For women who have had a hysterectomy (uterus removed).
- Combined HRT (Estrogen + Progestogen): Essential for women with a uterus. The progestogen protects the uterine lining from cancer risk associated with taking estrogen alone. This can be taken sequentially (causing a monthly bleed) or continuously (no bleed).
- Testosterone Therapy: Sometimes added in low doses to improve low libido, fatigue, or a reduced sense of well-being that persists despite other hormone therapy.
How is HRT Administered?
Modern HRT offers flexibility in how it’s delivered:
- Oral pills: Convenient but carry a slightly higher risk of blood clots as they are processed by the liver.
- Transdermal patches, gels, and creams: Applied to the skin, these deliver hormones directly into the bloodstream, bypassing the liver and lowering clot risk.
- Vaginal rings, creams, or tablets: Deliver low-dose estrogen directly to vaginal tissues to treat localized symptoms like dryness, with minimal systemic absorption.
- Implants: Small pellets inserted under the skin that release hormones over several months.
Who is a Good Candidate for HRT (and Who Isn’t)?
HRT is not for everyone. The decision depends on your symptoms and health profile.
Good candidates are generally healthy women under 60 (or within 10 years of menopause) whose symptoms disrupt their quality of life. It is also strongly recommended for women with premature or early menopause to protect against long-term health risks.
HRT is generally not recommended for women with a history of:
- Breast cancer or other hormone-sensitive cancers
- Blood clots (DVT or pulmonary embolism), stroke, or heart attack
- Active liver disease
- Undiagnosed vaginal bleeding
The Importance of Timing and Progestogen
Two concepts are crucial for safe and effective HRT:
- The “Timing Hypothesis”: Starting HRT within the “window of opportunity”—before age 60 or within 10 years of menopause—offers the best risk-benefit profile. Starting later increases cardiovascular risks.
- The Role of Progestogen: For women with a uterus, progestogen is not optional. It is an essential protective element that prevents estrogen from causing overgrowth of the uterine lining, which could lead to endometrial cancer. If you’ve had a hysterectomy, you don’t need it.
Understanding these principles is key to grasping the modern hrt meaning: replacing hormones the right way, at the right time, for your specific situation.
Exploring Alternatives and the HRT Meaning of ‘Bioidentical’
HRT is highly effective, but it’s not the only option. Whether HRT is unsuitable for you or you prefer to explore other paths, several alternatives exist. At ProMD Health, we support a holistic approach to menopausal health that includes lifestyle factors like diet and exercise, which can significantly help manage symptoms.
What is ‘Bioidentical’ Hormone Therapy?
The term “bioidentical” can be confusing. In the context of hrt meaning, it refers to hormones that are molecularly identical to those your body produces. They are often derived from plants (like soy or yams) and processed in a lab.
It’s crucial to understand the two types of bioidentical hormone therapy (BHRT):
- FDA-Approved BHRT: These are commercially manufactured and regulated products (like micronized progesterone and many forms of estradiol). They have been rigorously tested for safety, efficacy, and consistent dosing. Many conventional HRT products are, in fact, bioidentical.
- Custom-Compounded BHRT (cBHRT): These are mixed in special pharmacies and often marketed as “natural” or personalized. However, they are not FDA-approved and lack the same safety and efficacy testing. Major medical organizations advise against their use due to concerns about inconsistent dosing and a lack of robust scientific evidence. You can learn more from this evidence-based review of bioidentical hormones.
At ProMD Health, we prioritize evidence-based, FDA-approved bioidentical options when appropriate.
Non-Hormonal Alternatives for Symptom Management
If you can’t or don’t want to use hormones, you have effective options:
- Lifestyle Changes: A healthy diet, regular exercise, and stress reduction techniques (like yoga or meditation) can reduce hot flashes, improve mood, and protect bone health.
- Prescription Medications: Certain antidepressants (SSRIs/SNRIs), gabapentin, and clonidine can reduce hot flashes. A newer non-hormonal drug, fezolinetant, specifically targets the brain’s temperature-regulation center.
- For Vaginal Dryness: Over-the-counter vaginal moisturizers and lubricants are highly effective and safe for nearly everyone.
- Herbal Supplements: Phytoestrogens (from soy, flax) and black cohosh are used by some women, but scientific evidence for their effectiveness is mixed and inconsistent. Always discuss these with your provider, as even “natural” products can have side effects.
Frequently Asked Questions about HRT
Here are straightforward answers to some of the most common questions we hear from patients at ProMD Health.
How long can you safely stay on HRT?
There is no absolute time limit for taking HRT. The old “five years and you’re done” rule is outdated. The decision to continue or stop HRT is personal and should be based on an ongoing risk/benefit assessment with your doctor. The Menopause Society’s 2024 statement confirms that for healthy women with persistent symptoms, continuing HRT beyond age 65 can be a reasonable option, especially with lower doses and transdermal forms. The key is an annual check-up to reassess your needs and health status.
Does HRT cause weight gain?
No, HRT does not cause weight gain. The weight gain many women experience around menopause is due to natural metabolic changes, a slower metabolism, and loss of muscle mass that comes with aging and lower estrogen levels. This happens whether you take HRT or not. Some women may experience temporary bloating or water retention when first starting HRT, but this is not actual fat gain and usually resolves. A healthy diet and regular exercise remain the most effective tools for managing weight during this life stage.
Can I start HRT if I am over 60 or more than 10 years past menopause?
Based on the “timing hypothesis,” starting systemic HRT (pills, patches, gels) is generally not recommended for women over 60 or more than 10 years past menopause. Initiating therapy later in life is associated with an increased risk of cardiovascular events and stroke.
However, there is an important exception: local estrogen therapy for vaginal symptoms is safe and effective at any age. If your primary concerns are vaginal dryness, pain with intercourse, or recurrent UTIs, low-dose vaginal estrogen (creams, tablets, or rings) is an excellent option. It works directly where it’s needed with minimal absorption into the bloodstream, avoiding the risks of systemic HRT. As always, a thorough consultation is essential to determine the safest approach for you.
The Current Medical Consensus and Your Next Steps
After years of confusion, the medical consensus on HRT is now clear and reassuring: for most healthy, symptomatic women under 60 or within 10 years of menopause, the benefits of HRT generally outweigh the risks. Major medical organizations worldwide now recognize appropriately prescribed HRT as a safe and effective first-line treatment for managing menopausal symptoms.
The key is individualized care and shared decision-making between you and your healthcare provider. This is about finding what works for your body and your life.
The modern hrt meaning: A personalized approach
The modern hrt meaning is all about personalization. At ProMD Health, we create a plan by considering the whole picture: your specific symptoms, your personal and family medical history, your age and time since menopause, and your personal preferences and quality-of-life goals.
This is not a one-size-fits-all approach. We believe in shared decision-making, empowering you with knowledge about all your options—the benefits, risks, and alternatives. Treatment is reassessed annually to ensure it continues to serve you well as your body and needs evolve. HRT is often one piece of a comprehensive plan that includes nutrition, exercise, and stress management. You can learn more about our wellness services to see how we support your entire journey.
Finding More Information and Specialists
You don’t have to steer this journey alone. Excellent resources and expert support are available to guide you.
- The Menopause Society (formerly The North American Menopause Society) offers reliable, evidence-based information for women and provides a tool to find a menopause specialist in your area.
- Women’s Health Concern (part of the British Menopause Society) provides accessible, trustworthy information for women navigating menopause: https://www.womens-health-concern.org/
- Queer Menopause offers inclusive resources that address the unique experiences of queer and trans individuals: https://www.queermenopause.com/
Your most important resource is a qualified healthcare provider who listens and partners with you. At ProMD Health, our teams across Annapolis, Arlington, Ashburn, Bel Air, Bethesda, Columbia, Easton, Fort Lauderdale, Hutto, Lafayette, Lewes, Timonium, Tysons Corner, Washington, Wellington, and Westminster—and throughout Maryland, Virginia, Florida, Texas, Colorado, Delaware, and the District of Columbia—are trained in hormone optimization and comprehensive wellness care. We are committed to helping you maintain your vitality and confidence.
Understanding the true hrt meaning is the first step toward reclaiming your well-being. The second is reaching out for support. We invite you to schedule a consultation to explore how our services can help you feel like yourself again.