Estrogen deficiency symptoms: 1 Essential Guide
Understanding the Full Impact of Low Estrogen on Your Body
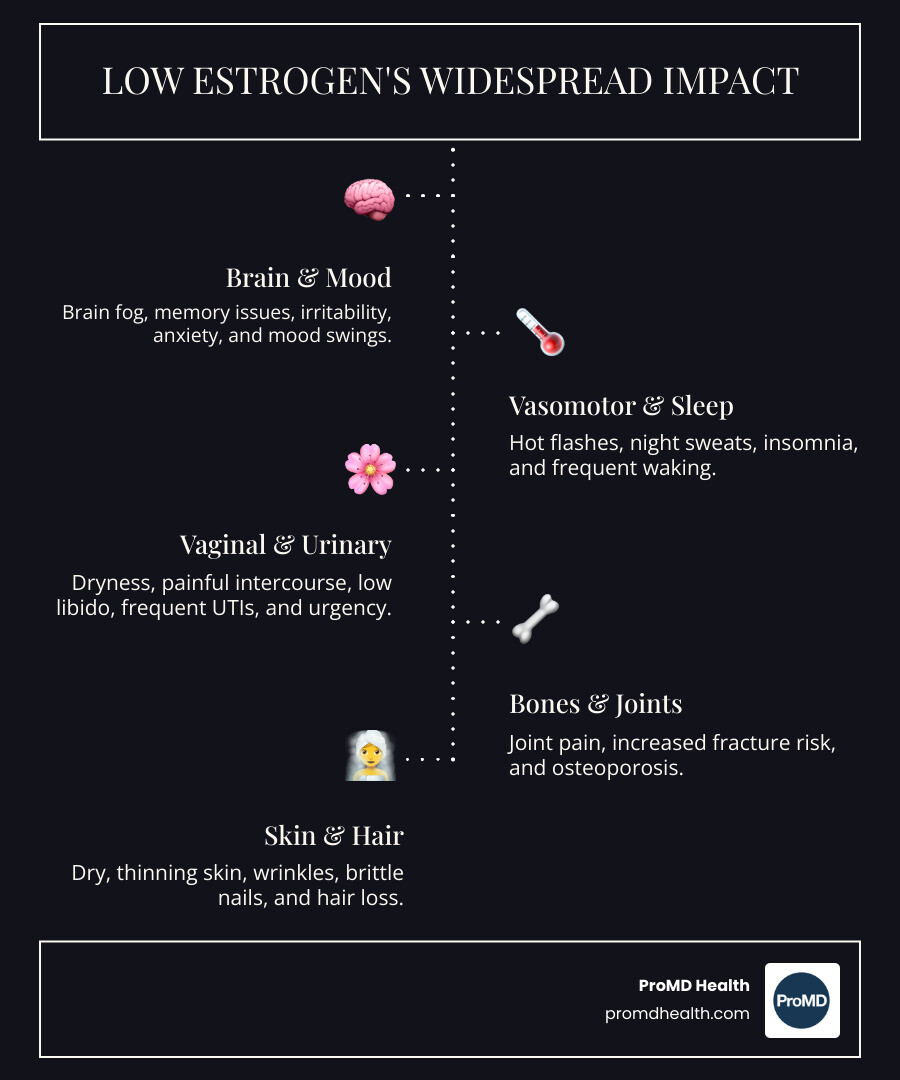
Estrogen deficiency symptoms affect far more than just your reproductive system. When estrogen levels drop, the effects ripple through nearly every part of your body—from your brain and bones to your skin and heart.
Common Estrogen Deficiency Symptoms Include:
- Vasomotor symptoms: Hot flashes and night sweats (affecting 40-80% of postmenopausal women)
- Sleep disturbances: Insomnia and frequent nighttime waking
- Mood changes: Irritability, anxiety, and mood swings
- Cognitive issues: Brain fog, memory problems, and difficulty concentrating
- Physical changes: Vaginal dryness, painful intercourse, and decreased libido
- Urinary problems: Frequent UTIs and urinary urgency
- Bone and joint health: Joint pain and increased fracture risk
- Skin and hair: Dry, thinning skin, wrinkles, and hair loss
- Weight changes: Unexplained weight gain, especially around the midsection
- Cardiovascular shifts: Changes in cholesterol and blood pressure
Many women don’t realize that their chronic joint pain, frequent bladder infections, or persistent brain fog could all stem from low estrogen. These symptoms often develop gradually during perimenopause—the years leading up to menopause—when estrogen levels begin their erratic decline. For some, symptoms last just a year or two. For others, they persist for several years or longer.
The good news? Understanding these symptoms is the first step toward finding relief. Whether through hormone therapy, lifestyle modifications, or a combination of approaches, effective treatments exist to help you feel more like yourself again.
As Scott Melamed, President and CEO of ProMD Health with extensive training in biotechnology from Johns Hopkins University, I’ve seen how recognizing estrogen deficiency symptoms early can transform a patient’s quality of life. Our multidisciplinary approach helps patients steer these hormonal changes with evidence-based, personalized care.
What is Estrogen and Why is it So Important?
Estrogen is often called the “headline hormone” in the female body, and for good reason. It’s not just one hormone, but a group of sex hormones produced primarily in the ovaries. It plays a vital role in women’s reproductive health, but its influence extends far beyond that, affecting nearly every system in the body.
There are three main types of estrogen, each with distinct roles:
- Estradiol (E2): This is the most potent form of estrogen and is the primary estrogen during a woman’s reproductive years. It’s crucial for the development of female sexual characteristics and maintaining the reproductive system.
- Estrone (E1): This is the main estrogen found in women after menopause. It’s weaker than estradiol and is primarily produced in fat cells rather than the ovaries.
- Estriol (E3): This is the primary estrogen during pregnancy, produced in large amounts by the placenta.
The widespread impact of estrogen is due to the presence of estrogen receptors throughout the body, including in our bones, heart, brain, skin, and even our digestive system. This means that when estrogen levels are healthy, it supports:
- Reproductive Health: Estrogen regulates the menstrual cycle, promotes the growth of the uterine lining, and is essential for fertility.
- Bone Density: Estrogen is vital for maintaining strong bones by preventing calcium loss. Without enough estrogen, our bones can become weak and brittle.
- Cardiovascular Protection: Estrogen can positively impact heart and blood vessel health, for example, by influencing cholesterol levels and blood pressure.
- Brain Function: It plays a role in mood, cognitive function, and even memory.
- Skin and Hair Health: Estrogen contributes to skin hydration, collagen production, and hair follicle health.
For more scientific research on estrogen’s functions, you can refer to resources like the Endocrine Society’s infographics: scientific research on estrogen’s functions.
The Normal Fluctuation of Estrogen
Estrogen levels are dynamic, constantly rising and falling throughout a woman’s life. During the reproductive years, these fluctuations are most noticeable as part of the menstrual cycle. For instance, after ovulation, estrogen levels are typically high as the uterine lining thickens in preparation for a potential pregnancy. If pregnancy doesn’t occur, estrogen levels drop, leading to menstruation. You can learn more about these fluctuations during the menstrual cycle here: ovulation and estrogen peaks.
Pregnancy brings significantly higher estrogen levels to support the growing fetus. After giving birth, estrogen levels rapidly decrease to pre-pregnancy levels, which can contribute to postpartum mood changes and other symptoms.
However, the most significant and sustained drop in estrogen occurs during the menopausal transition.
Perimenopause vs. Menopause: The Estrogen Decline
It’s important to distinguish between perimenopause and menopause, as they represent different stages of estrogen decline.
Perimenopause is the transitional period leading up to menopause. During this time, which can last several years, our ovaries gradually begin to produce less estrogen. This decline isn’t a smooth, steady decrease; instead, estrogen levels can fluctuate wildly, leading to a wide array of symptoms. It’s like a hormonal rollercoaster, with unpredictable highs and lows. Many of the initial estrogen deficiency symptoms begin during perimenopause.
Menopause, on the other hand, is officially diagnosed after 12 consecutive months without a menstrual period, not due to other causes. At this point, the ovaries have largely stopped producing estrogen, leading to consistently low levels of the hormone. The average age for menopause is around 52, but it can occur earlier or later. The long-term health implications of consistently low estrogen become more pronounced after menopause.
Understanding the Wide-Ranging Estrogen Deficiency Symptoms
When we talk about estrogen deficiency symptoms, many people immediately think of hot flashes. While hot flashes are a hallmark symptom, they are just one piece of a much larger puzzle. Estrogen’s widespread influence means that a deficiency can impact virtually every system in your body, often leading to surprising and sometimes subtle symptoms that are easily overlooked or misattributed.
The variability of these symptoms is also notable. One woman might experience severe hot flashes but no cognitive issues, while another might struggle with joint pain and brain fog, with only mild hot flashes. The duration of symptoms also varies; some may find relief within a year or two, while others contend with symptoms for many years.
Common Estrogen Deficiency Symptoms You Might Expect
Let’s start with the more widely recognized estrogen deficiency symptoms:
- Hot Flashes and Night Sweats: These are perhaps the most iconic symptoms. Hot flashes involve a sudden, intense feeling of heat, often accompanied by sweating and flushing. When they occur during sleep, they’re called night sweats and can severely disrupt sleep. Statistics show that 40% to 80% of postmenopausal women report experiencing hot flashes. In most cases, these vasomotor complaints last for at least 1 to 2 years, but for a significant number of women, they can persist for much longer.
- Irregular Periods: During perimenopause, as estrogen levels become erratic, menstrual cycles can become unpredictable—shorter, longer, lighter, heavier, or simply skipping months.
- Vaginal Dryness and Pain During Intercourse (Dyspareunia): Estrogen is crucial for maintaining the health, elasticity, and lubrication of vaginal tissues. As levels drop, these tissues can become thinner, drier, and more fragile, leading to discomfort, itching, and pain during sexual activity.
- Low Libido: A decreased sex drive is a common complaint with low estrogen, often compounded by the physical discomfort of vaginal dryness. You can find more information about low estrogen and decreased libido here: Low libido.
- Mood Swings, Irritability, and Fatigue: Estrogen plays a role in regulating neurotransmitters like serotonin, which influence mood. Fluctuating or low levels can lead to increased irritability, anxiety, sadness, and unpredictable mood swings. When combined with disrupted sleep from night sweats, fatigue can become profound, further exacerbating mood issues.
Lesser-Known Estrogen Deficiency Symptoms to Watch For
Beyond the usual suspects, many estrogen deficiency symptoms are less commonly discussed but can significantly impact daily life. These are the subtle clues your body might be sending:
- Sleep Disturbances and Insomnia: Estrogen helps regulate body temperature and brain function related to sleep. Low estrogen can interfere with our sleep architecture, leading to difficulty falling asleep, staying asleep, or experiencing restless sleep. Even if you don’t have night sweats, you might find yourself waking up tired, struggling to get the recommended seven to nine hours of sleep each night.
- Frequent Urinary Tract Infections (UTIs) and Bladder Changes: The tissues of the urinary tract, like the vagina, are estrogen-dependent. When estrogen is low, the lining of the urethra and bladder can become thinner and less elastic. This can make us more susceptible to UTIs, urinary urgency, and even incontinence. It’s a common,, link between hormones and bladder health.
- Skin Changes (Dryness, Wrinkles, Thinning): Estrogen plays a vital role in maintaining skin health by supporting collagen production, elasticity, and hydration. With low estrogen, you might notice your skin becoming unusually dry, itchy, or less plump, even with your usual moisturizers. This can lead to increased fine lines and wrinkles. Some even refer to a “low estrogen face” characterized by duller, thinner skin with more wrinkles.
- Hair Thinning and Brittle Nails: Just as estrogen affects skin, it also impacts hair follicles and nail strength. You might observe your hair becoming thinner, losing its luster, or your nails becoming more brittle and prone to breakage.
- Joint Pain (Arthralgia): Estrogen has anti-inflammatory properties and plays a role in maintaining cartilage and joint lubrication. Many women report new or worsening aches, stiffness, or pain in their joints, such as knees, hips, or fingers, as estrogen levels decline. This is why we often hear patients say they feel like they’re “falling apart” during perimenopause.
- Cognitive Changes (Brain Fog, Memory Issues): Estrogen supports various brain functions, including memory, focus, and verbal fluency. When levels drop, many women experience “brain fog,” difficulty concentrating, forgetfulness, or a general feeling of mental sluggishness. It can be frustrating to feel like your brain isn’t as sharp as it used to be.
- Weight Gain (Especially Abdominal): Despite maintaining diet and exercise, many women experience unexplained weight gain, particularly around the midsection, during perimenopause and menopause. Estrogen influences metabolism and fat distribution, and its decline can shift where our bodies store fat.
- Headaches or Migraines: For some women, a drop in estrogen can trigger more frequent or severe headaches and migraines. If you’ve always been prone to hormonal headaches, you might notice them intensifying during this transition.
These lesser-known estrogen deficiency symptoms can be confusing because they often mimic other conditions or are simply dismissed as “getting older.” That’s why understanding the full spectrum of estrogen’s influence is so crucial.
What Causes Estrogen Levels to Drop?
While menopause is the most common and widely recognized cause of declining estrogen, several other factors can lead to estrogen deficiency symptoms.
- Menopause and Ovarian Function Decline: As we age, our ovaries naturally become less responsive and produce fewer hormones, including estrogen. This gradual decline marks the perimenopausal transition, eventually leading to menopause when ovarian function ceases.
- Premature Menopause or Primary Ovarian Insufficiency (POI): Some women experience menopause before the age of 40 (premature menopause) or 45 (early menopause). Primary ovarian insufficiency (POI) occurs when ovaries stop functioning normally before age 40. This can be due to genetic factors, autoimmune diseases, or unknown causes.
- Surgical Menopause (Oophorectomy): The surgical removal of one or both ovaries immediately halts estrogen production, leading to an abrupt and often more severe onset of estrogen deficiency symptoms.
- Pituitary Gland Conditions: The pituitary gland, located in the brain, produces hormones that signal the ovaries to produce estrogen. Disorders of the pituitary gland, such as hypopituitarism, can disrupt this signaling, leading to low estrogen levels. You can learn more about pituitary gland disorders here: pituitary gland.
- Cancer Treatments: Chemotherapy and radiation therapy, especially to the pelvic area, can damage the ovaries and significantly reduce estrogen production, sometimes leading to temporary or permanent menopause.
- Chronic Stress: Research shows that chronic stress can reduce estrogen levels. Our bodies prioritize stress hormones like cortisol during periods of high stress, which can impact the production of other hormones. Find out more about the impact of stress on estrogen levels here: Chronic stress impact.
- Excessive Exercise and Eating Disorders: Conditions like hypothalamic amenorrhea, often seen in female athletes or individuals with eating disorders, result from insufficient caloric intake and/or excessive exercise. This puts stress on the body, signaling the hypothalamus to reduce hormone production, including estrogen, leading to absent periods.
- Certain Medications: Some medications, particularly those used in cancer treatment (like aromatase inhibitors), can intentionally lower estrogen levels.
- Exposure to Endocrine-Disrupting Chemicals (EDCs): These ubiquitous chemicals, found in plastics, packaging, nonstick pans, and fragrances, can mimic estrogen or act as anti-estrogens, negatively affecting hormonal balance. While the exact cause-and-effect relationship is still being researched, studies support a link between EDCs and harm to human health. Learn more about EDCs here: Exposure to endocrine-disrupting chemicals.
Long-Term Health Risks of Estrogen Deficiency
The impact of low estrogen extends beyond uncomfortable daily symptoms; it poses significant long-term health risks that can affect our quality and quantity of life. Addressing estrogen deficiency symptoms is not just about comfort, but about protecting our future health.
- Osteoporosis: Estrogen is a key player in maintaining bone density. It helps regulate the balance between bone formation and bone resorption, ensuring our bones remain strong. When estrogen levels decline, bone loss accelerates, leading to osteopenia (reduced bone density) and eventually osteoporosis, a disease that makes bones brittle and prone to fractures. This is a significant concern, as osteoporosis affects about one in five women over 50 in the United States. You can find this statistic here: Osteoporosis statistic (one in five women over 50). The most rapid bone loss often occurs in the three years surrounding menopause.
- Heart Disease: Before menopause, women generally have a lower risk of heart disease compared to men. Estrogen is thought to play a protective role by influencing cholesterol levels (raising HDL or “good” cholesterol), maintaining blood vessel elasticity, and reducing inflammation. After menopause, as estrogen levels drop, our risk for heart disease rises sharply. This can involve changes in blood pressure, cholesterol levels, and increased inflammation. Understanding cardiovascular risks in menopause is crucial: Cardiovascular risks in menopause.
- Genitourinary Syndrome of Menopause (GSM): This is a comprehensive term for the collection of symptoms affecting the lower urinary tract and genital organs due to estrogen deficiency. It includes vaginal dryness, burning, irritation, painful intercourse, urinary urgency, painful urination, and recurrent urinary tract infections. Untreated, these symptoms can significantly impact quality of life and sexual health.
- Cognitive Decline: While “brain fog” is an acute symptom, chronic estrogen deficiency may contribute to long-term cognitive decline. Estrogen’s neuroprotective effects and its role in brain function suggest that its absence could impact memory, executive function, and potentially increase the risk of neurodegenerative diseases.
Diagnosis and Management of Low Estrogen
If you suspect you’re experiencing estrogen deficiency symptoms, the first and most important step is to consult a healthcare provider. We believe in a thorough, personalized approach to diagnosis and management.
Our process typically begins with:
- Symptom Evaluation: We’ll discuss your symptoms in detail, including their onset, severity, and impact on your daily life. It’s helpful to track your symptoms and any patterns you notice.
- Medical History: A comprehensive review of your medical history, including menstrual cycles, pregnancies, past medical conditions, and medications, provides crucial context.
- Physical Exam: A physical examination helps us assess your overall health and identify any physical signs of estrogen deficiency.
- Blood Tests: To confirm low estrogen levels and rule out other conditions, we often recommend simple blood tests. These can measure:
- Estrogen levels: Specifically estradiol (E2), which is the most common form of estrogen tested. We may also look at estrone (E1).
- Follicle-Stimulating Hormone (FSH): High FSH levels typically indicate that the ovaries are no longer responding to signals from the brain to produce estrogen, a common sign of perimenopause or menopause.
- Other hormone levels (e.g., thyroid, progesterone) may also be checked to get a complete picture of your hormonal health.
Once a diagnosis of low estrogen is confirmed, we work with you to develop a personalized treatment plan.
Medical Treatments: Understanding Hormone Therapy (HT)
Hormone Therapy (HT), also known as Menopausal Hormone Therapy (MHT), is the most effective treatment for many estrogen deficiency symptoms, particularly hot flashes and vaginal dryness. HT involves replacing the hormones your body is no longer producing.
There are different types of HT:
- Estrogen-Only Therapy (ET): This is typically prescribed for women who have had a hysterectomy (surgical removal of the uterus).
- Combined Estrogen-Progestin Therapy (EPT): For women who still have their uterus, estrogen is combined with progesterone (or a synthetic progestin). This is crucial because estrogen alone can stimulate the growth of the uterine lining, increasing the risk of uterine cancer. Progesterone protects the uterus from this overgrowth.
The benefits of HT can be significant:
- Symptom Relief: HT is highly effective in reducing hot flashes, night sweats, and vaginal dryness.
- Bone Protection: It helps prevent bone loss and reduces the risk of osteoporosis and fractures.
- Improved Quality of Life: By alleviating disruptive symptoms, HT can improve sleep, mood, and overall well-being.
However, understand the potential risks of HT, which vary depending on individual health factors, the type of hormones used, the dosage, and the duration of treatment. Risks can include a slightly increased risk of blood clots, stroke, and certain cancers (like breast cancer with long-term combined EPT). The latest research on hormone therapy continues to evolve, helping us understand the nuances of risks and benefits: Latest research on hormone therapy.
HT can be delivered in various ways:
- Systemic Estrogen: These forms (pills, patches, gels, sprays) deliver estrogen throughout the body, treating systemic symptoms like hot flashes and protecting bones.
- Local Estrogen: These forms (vaginal creams, tablets, rings) deliver estrogen directly to the vaginal tissues. They are highly effective for treating vaginal dryness and genitourinary symptoms with minimal systemic absorption, making them a safer option for many.
At ProMD Health, we prioritize a precision medicine approach, considering your specific genes, environment, and lifestyle to tailor hormone therapy to your unique needs. We offer various bioidentical hormone replacement options, which are biochemically identical to the hormones your body naturally produces. This personalized approach helps us optimize results and minimize risks.
Lifestyle and Natural Approaches to Manage Symptoms
While medical treatments like HT are highly effective, lifestyle modifications and natural approaches can complement therapy or provide relief for milder estrogen deficiency symptoms.
- Dietary Changes:
- Phytoestrogens: Incorporating foods rich in phytoestrogens, plant compounds that mimic estrogen’s effects, may help. Examples include soy products (tofu, tempeh), flaxseeds, legumes, and certain berries.
- Calcium and Vitamin D: These are crucial for bone health. Ensure adequate intake through diet or supplements, especially when estrogen is low. Consulting a registered dietitian can provide individualized nutritional strategies: registered dietitian.
- Balanced Nutrition: Maintaining a healthy diet rich in fruits, vegetables, and whole grains supports overall health and hormonal balance. Avoid excessive calorie restriction, which can exacerbate low estrogen.
- Regular Exercise: Moderate, consistent exercise, including weight-bearing activities, is beneficial for bone health, mood, and weight management. However, excessive exercise can sometimes lower estrogen levels, so finding a balance is key.
- Stress Management: Chronic stress can negatively impact hormone balance. Techniques like yoga, meditation, deep breathing exercises, and spending time in nature can help reduce stress levels.
- Sleep Hygiene: Prioritize getting 7-9 hours of quality sleep each night. Establish a regular sleep schedule, create a relaxing bedtime routine, and optimize your sleep environment to address sleep disturbances.
- Limiting Alcohol and Caffeine: These can exacerbate hot flashes and disrupt sleep for some individuals.
- Quitting Smoking: Smoking has numerous negative health impacts and can worsen menopausal symptoms.
- Reducing Exposure to Endocrine-Disrupting Chemicals: While these are everywhere, making conscious choices to avoid certain plastic containers, canned foods, and products with synthetic fragrances can help support hormonal health.
Conclusion: Taking Control of Your Hormonal Health
We’ve explored how estrogen, the “headline hormone,” impacts far more than just reproductive health, influencing everything from our mood and sleep to our bones and skin. We’ve digd into the common and lesser-known estrogen deficiency symptoms, from the classic hot flashes and mood swings to surprising joint pain and frequent UTIs. Understanding the various causes, from the natural decline of menopause to lifestyle factors and environmental influences, is the first step toward regaining control.
The long-term health risks associated with untreated low estrogen, such as osteoporosis and heart disease, underscore the importance of addressing these changes proactively.
The good news is that you don’t have to suffer in silence. With a personalized approach to diagnosis and management, including medical treatments like Hormone Therapy (HT) and supportive lifestyle modifications, relief is possible. Our team at ProMD Health, with locations in Annapolis, Arlington, Ashburn, Bel Air, Bethesda, Columbia, Easton, Fort Lauderdale, Hutto, Lafayette, Lewes, Timonium, Tysons Corner, Washington, Wellington, and Westminster, is here to guide you. We combine advanced medical knowledge with a warm, empathetic approach to help you steer these hormonal shifts.
If you’re experiencing persistent or concerning estrogen deficiency symptoms, it’s time to seek medical advice. Don’t let these symptoms diminish your quality of life. Empower yourself with knowledge and partner with healthcare professionals who understand the complexities of hormonal health.
Taking the next step toward feeling younger and living your best life starts with understanding your body. We invite you to explore how our hormone optimization therapy can help you regain your equilibrium and vitality.